Pros and Cons of Outsourcing Benefit Administration

Employers may feel that keeping up with employee benefits management is often a time-consuming and complex task, with several daily challenges for human resources (HR) leaders to navigate. If this sounds like your experience, you’re not alone. Benefit administration demands significant time and attention to be done right, yet it’s an essential responsibility that’s vital for keeping your employees happy and healthy.
For many employers, especially with small business medical benefits, the questions keep piling up: How can we better support our employees while still managing costs? How can we ensure our business stays compliant with changing regulations? What happens if we make a mistake? These concerns, combined with juggling compliance, support, and rising costs, have left many employers looking to rethink their approach to employee health benefits administration.
If you’re looking for a better way to manage employee benefits, you might consider one potential solution: outsourcing benefits administration. In this article, we’ll explore what outsourced benefit administration involves, whether it’s right for your business, and show you how Vitable is simplifying benefits management while keeping your employees’ best interests at heart.
Key takeaways from this article:
- Understand what outsourced benefits administration means, what it includes, and how it supports HR operations.
- Learn the real-world pros and cons of outsourcing—from time and cost savings to potential challenges with control and employee experience.
- From ICHRA and QSEHRA to DPC, discover how Vitable’s all-in-one healthcare solution can streamline benefit administration, reduce administrative burden, and elevate care for your workforce.
Continue reading to understand the pros and cons of outsourcing benefit administration and learn how Vitable can help your business streamline its approach to employee benefits.
What is Benefit Administration?
Benefit administration involves comprehensively managing the company’s employee benefits programs. Typically, this is led by the HR department, and the organization’s finance and operations teams also help with budgeting and implementation. Effectively, you can think of benefit administration as the crucial process of taking care of your employees’ health and wellness through its four key core functions.
- Plan selection and enrollment: Employers must carefully choose their health benefits packages while helping employees get onboarded during open enrollment periods.
- Employee communications and education: Employers are responsible for ensuring employees understand which benefits are available to them and how to make the most of them. This is done through ongoing communication and education initiatives.
- Compliance with health regulations: Benefits administrators must stay up-to-date with important healthcare and benefits regulations, such as the Affordable Care Act (ACA), Health Insurance Portability and Accountability Act (HIPAA), and Consolidated Omnibus Budget Reconciliation Act (COBRA), to keep the company and its employees protected.
- Ongoing support and issue resolution: With any benefits-related questions or issues that may come up, benefits administration must provide ongoing support and resolution in a timely manner.
Why does it matter to get benefits administration right? Because with the right approach, employers can show their employees that they are highly valued by the company. Employer-provided health benefits are consistently a top priority for workers in the US. By ensuring your workforce is well-cared for through comprehensive benefits, they're more likely to stay with your company and feel satisfied with their jobs.
Effective benefits administration also protects the company legally by ensuring compliance with key healthcare laws (e.g., ACA, HIPAA, etc.), while boosting cost savings and productivity long-term by increasing employee retention. Examples of highly coveted benefits include health benefits, paid time off (PTO), ancillary coverage (e.g., vision and dental), paid leave programs for pregnancy and parenthood, and flexible work schedules, among others.
What is Outsourced Benefit Administration?
According to the 2024 Deloitte Global Outsourcing survey, 57% of companies were outsourcing their HR activities, including benefit administration. When employers rely on outsourced benefit administration, they delegate part or all of the business’s employee benefits management to a specialized third-party benefits provider. These external partners are experts in benefit administration, taking on all core day-to-day responsibilities like coordinating employee payroll and benefits processes, monitoring company compliance with the latest regulations, and providing continuous support to your employees.
Other important benefits-related duties that can be delegated to third-party benefits partners include:
- Administering retirement benefit programs, such as 401(k) or pension plans
- Tracking and managing employee PTO
- Managing coverage through an Individual Coverage Health Reimbursement Arrangement (ICHRA) or Qualified Small Employer HRA (QSEHRA) for medical, dependent care, or other expenses
- Developing initiatives to promote employee health and well-being
- Managing the enrollment process
- Completing claims processing
By outsourcing to these experts, employers can also take advantage of the provider’s existing infrastructure for efficient employee benefits communication to ensure workers are actually using the benefits available to them. Benefits administrator companies also often bring their own user-friendly enrollment tools that make it easier for employees to learn about what perks are offered and how to sign up for them. They may also offer cost reporting and analysis, delivering regular reports on benefits, costs, and usage.
Certainly, this arrangement can significantly simplify employee benefits management, but it’s also important to remember that outsourcing benefit administration does not mean employers relinquish any control over crucial business choices. Ultimately, you still have full authority and oversight on plan selection and strategic decision-making, while the day-to-day administrative tasks are left to be handled by your external benefits partner.

Download 2025 Employer Guide to ICHRA
Vitable’s ICHRA Guide gives employers a clear, step-by-step resource for building smarter, ACA-compliant benefits.
This guide explains how ICHRAs work, who qualifies, and how Vitable simplifies setup, onboarding, reimbursements, and compliance — while giving employees more flexibility, control, and care.
Download Vitable’s 2025 Broker’s Guide to ICHRA
The Broker Guide to ICHRAs is a comprehensive resource that helps brokers understand, sell, and manage Individual Coverage HRAs with confidence.
This guide covers everything from compliance and class design to administration flows, case studies, and how Vitable streamlines quoting, enrollments, and reimbursements for brokers, employers, and employees.
Pros of Outsourcing Benefit Administration
Now that we’ve covered the basics of benefit administration and what it means for employers to outsource these tasks, let’s explore five key advantages of partnering with a specialized benefits provider.
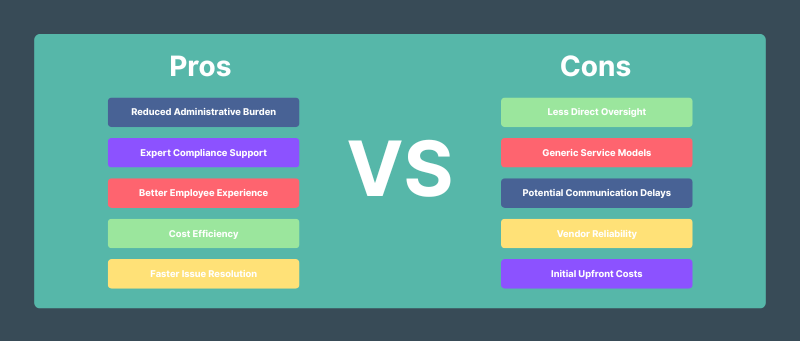
1. Reduced Administrative Burden
First and foremost, regardless of the size of your company, outsourced benefit administration significantly reduces the administrative burden on your HR team. By delegating out day-to-day benefits-related duties to these external partners, your company’s HR department can dedicate more time and resources to developing strategic initiatives to help grow your business and support employee engagement.
2. Expert Compliance Support
External benefits administrators are experts when it comes to employee health benefits management and compliance. Employers can have the peace of mind knowing their benefits programs will be able to keep up with the latest healthcare regulations and complex legal requirements, while ensuring the business is audit-ready.
3. Better Employee Experience
Another key advantage is that employers can provide a better employee experience when benefits management is outsourced. Because these external providers already have a robust infrastructure to support employees, they provide easy access to faster support through dedicated service teams, convenient centralized benefit access through user-friendly online platforms, and clear resources to help them better understand their options. These services can improve employee satisfaction and loyalty, work productivity, long-term retention, and the company’s ability to attract top talent in the job market.
4. Cost Efficiency
From a financial perspective, outsourcing benefits administration might come with upfront set-up costs, but in the long run, it typically results in significant savings for employers from improved efficiency and lower administrative overhead. That is, employee benefits management is complex and involves several moving pieces, but external providers already have built-in systems to handle these tasks efficiently. Employers also have access to the vendor’s long-standing expertise in benefit administration at affordable costs, eliminating the need to hire and train in-house benefits specialists, while reducing administrative burden on their HR team.
5. Faster Issue Resolution
Lastly, outsourcing to companies like Vitable allows employers and their HR teams to stress less about any benefits-related issues or questions that may arise. Partnering with specialized benefit administrators provides continuous access to trained benefit specialists who are ready to help solve problems quickly. This results in a smoother experience for both employers and employees alike.
Other advantages to look forward to with outsourcing benefit administration include greater scalability and flexibility as your company grows and its needs change, robust data privacy and security processes, and a simplified open enrollment experience, allowing your HR team to focus more on employee engagement during this period.
Cons of Outsourcing Benefit Administration
Despite its several advantages, there are also some important drawbacks to consider before determining whether outsourcing benefit administration is the right approach for your business.
1. Less Direct Oversight
First, employers may have less direct control and insights into how your employee benefits program is managed day-to-day. Although this certainly reduces administrative burden for the HR team, it also means they may not identify potential problems as quickly as they would with in-house benefits specialists.
2. Generic Service Models
Depending on which third-party benefits providers you choose, they may use a generic one-size-fits-all service approach that is not uniquely tailored to your company’s culture or needs.
3. Communication Delays
Outsourcing itself also comes with some common pitfalls that must be anticipated and prepared for prior to starting the partnership. Primarily, working with a third-party vendor can introduce communication delays, with slower response times or problem resolution than with in-house management. Without establishing proper channels of communication, your employees may have to wait longer to get their benefits-related questions answered.
4. Vendor Reliability
The reputation and reliability of the benefits provider that your company chooses are other critical factors to keep in mind. If they’re unable to meet your business’s employee health benefits management needs, this will potentially create more complications for the HR team, decrease administrative efficiency, and even negatively impact employee satisfaction.
5. Initial Costs
Finally, as we mentioned earlier, outsourcing your employee benefits management will require upfront investments before your company can reap the benefits. This means your business will need to carefully budget for new short-term costs, such as system set-up and integration, as well as employee training and onboarding.
Is Outsourcing Right for Your Business?
In addition to weighing the key pros and cons we covered here, there are also several important factors for employers to consider before deciding whether outsourcing benefits administration is right for them. Here are the most crucial ones to remember.
- Workforce Size:
How many employees does your company have? For larger organizations that are managing benefits for more people, outsourcing may make the most sense.
- Internal HR Capacity and Expertise:
If your HR team is already at capacity with their current tasks or if they lack specialized benefits expertise, outsourcing to external professionals can significantly streamline employee benefits management.
- Budget Limitations:
Depending on the financial capabilities of your business, it is important to review your budget and determine whether the long-term savings from outsourcing will outweigh the upfront costs required.
- Regulatory Complexity:
How familiar is your HR team with the current landscape of healthcare and benefits regulations? Depending on these needs, turning to a specialized external provider may provide better protections for your business and employees through comprehensive regulatory compliance monitoring.
- Number of Benefit Offerings:
How complex are your benefit offerings? The more services that require oversight and management, the more helpful outsourcing to benefits experts may be.
Overall, outsourced benefit administration offers the most strategic advantages for certain business scenarios. For example, fast-growing companies can rely on outsourcing to scale their employee health benefits management without having to hire and train more HR staff. In cases of mergers and acquisitions, an external administrator can also help combine each organizations’ benefits offerings into one harmonized program.
Additionally, businesses with high employee turnover or smaller HR teams that are stretched thin may face greater administrative burdens. In these scenarios, outsourcing to a third party can keep your benefits program running smoothly, allowing your team to focus on growing the company and supporting employees.
Vitable: A Better Way to Manage Health Benefits
Vitable is a health benefits platform built to make care better for everyday workers—and simpler for the teams who support them. We partner with employers to streamline health benefits administration through flexible, ACA-compliant coverage options designed to improve access, reduce costs, and lighten the administrative load.
By relying on Vitable for outsourced health benefit administration, employers can choose from several flexible, regulatory-compliant coverage packages, including ICHRA and QSEHRA options and Minimum Essential Coverage (MEC) + Minimum Value Plans. If you’re an applicable large employer, we’ll also help you stay ACA-compliant with solutions tailored to your workforce and budget. We can guide you on how to leverage ICHRA or other HRA solutions for ACA compliance in 2025.
Each Vitable plan comes standard with our built-in Direct Primary Care (DPC) membership, giving employees access to same-day or next-day visits, virtual and in-home care, and no copays or deductibles. See how DPC works with MEC to support compliance while offering better care.
Why HR Teams Love Vitable:
- Built-In Compliance
- Stay ACA- and IRS-compliant without adding more to your HR team’s plate.
- DPC Membership, Included
- Employees get high-quality primary care with no copays, no deductibles, and no insurance claims.
- Centralized Platform
- Manage enrollment, education, and compliance in one place—no more juggling vendors or systems.
- Real Support, Real People
- Get fast answers and expert help from dedicated Vitable specialists. No call center headaches.
Ready for better health benefits administration for your business? Let Vitable handle the heavy lifting so you can focus on what matters most: building a better workplace for your team. Visit our website to learn more or book a free consultation today!
Ready to learn more?
Stay ahead with the latest insights on healthcare, benefits, and compliance—straight to your inbox.
Get a quote
Get a personalized health benefits quote tailored to your company’s unique needs.
Vitable helps employers provide better healthcare to their employees and dependents by improving accessibility, cost, and quality.
